Tests and Exams
Doctors normally diagnose tinea pedis or athlete’s foot by observing your feet. Your doctor may also ask questions about the symptoms and your history of fungal infections. If you have unusual symptoms, or in case previous fungal infections have not healed completely, the doctor may scratch the skin or trim a nail to take a sample for examination. The doctor may use laboratory tests such as potassium hydroxide (KOH) preparation and fungal culture to check the existence of the fungus and determine the nature of the identified fungus. In rare situations, the doctor may use skin biopsy, which involving extracting some skin from the infected part and using a microscope to examine it.
Treatment Overview
 The severity and type of tinea pedis determine how you should treat the condition. Home treatment with antifungal medications can treat most instances of tinea pedis. Antifungal medications either kill the fungi or prevent them from growing. Nonprescription antifungal medications are usually the first modes of treatment for tinea pedis. The common nonprescription drugs for athlete’s foot include clotrimazole, terbinafine, miconazole, and tolnaftate. All of them are topical medications meaning that they should be applied externally. Prescription drugs are used when nonprescription antifungals fail to treat the condition or in case of severe infections. Topical prescription medications for athlete’s foot include clotrimazole, butenafine, and naftifine. Oral prescription antifungal medications include itraconazole, fluconazole, and terbinafine.
The severity and type of tinea pedis determine how you should treat the condition. Home treatment with antifungal medications can treat most instances of tinea pedis. Antifungal medications either kill the fungi or prevent them from growing. Nonprescription antifungal medications are usually the first modes of treatment for tinea pedis. The common nonprescription drugs for athlete’s foot include clotrimazole, terbinafine, miconazole, and tolnaftate. All of them are topical medications meaning that they should be applied externally. Prescription drugs are used when nonprescription antifungals fail to treat the condition or in case of severe infections. Topical prescription medications for athlete’s foot include clotrimazole, butenafine, and naftifine. Oral prescription antifungal medications include itraconazole, fluconazole, and terbinafine.
In case severe cases of tinea pedis do not improve, the doctor can prescribe pills or oral antifungal drugs. Oral medications are prescribed for severe infections because of their high costs and the need for periodic testing to identify undesired side effects. Tinea pedis may reoccur even after this treatment. Always complete the prescribed dosage even if the condition improves or heals soon after you start using medication. The aim is to prevent the condition from returning. Given that there are chances of reinfection, any symptoms of the condition should be treated completely.
Web Infections on Toes
Toe web or interdigital infection affects the area between your toes. It is a common tinea pedis infection that mostly affects the 4th and 5th toes. You can treat mild and moderate cases of this infection by cleaning and drying your feet regularly. You can also use nonprescription antifungal lotions and ointments. In severe cases of the infection, your physician can prescribe topical or oral antifungal or antibiotic medications.
Moccasin-type Tinea Pedis
 People who have this infection have a thick and scaly skin on their heels and soles. This infection usually affects the toes and is known as onychomycosis. It is hard to treat this infection because of the thickened skin. For example, it is difficult for nonprescription medicines to penetrate the skin. Use prescription antifungal medications that can penetrate the skin like ketoconazole. Prescription oral medications can also treat the condition.
People who have this infection have a thick and scaly skin on their heels and soles. This infection usually affects the toes and is known as onychomycosis. It is hard to treat this infection because of the thickened skin. For example, it is difficult for nonprescription medicines to penetrate the skin. Use prescription antifungal medications that can penetrate the skin like ketoconazole. Prescription oral medications can also treat the condition.
Vascular Infections
These infections occur in the instep, sole, heel, toes, and on the upper side of your foot. People with this condition may also acquire bacterial infections. Treatment can be carried out at home or at the doctor’s office. The physician removes the blister tops and soaks the feet until the affected area dries. At home, dry the blisters by soaking the feet in Burow’s solution more than a few times daily for at least three days. Apply a topical antifungal ointment after the soaked area dries out. Additionally, use oral antibiotics if you have bacterial infections. Apart from antifungal pills and creams, the physician may recommend corticosteroid pills.
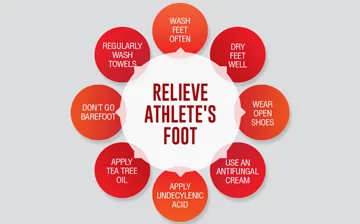
Prevention
 Athlete’s foot usually returns due to the lack of preventive measures, failure to use antifungal medications as required and resistant fungi that fail to disappear even after thorough treatment. You can inhibit the condition by drying your feet after coming into contact with water, wearing open-toed shoes, wearing sock indoors, changing socks, wearing socks that can absorb sweat, using antifungal powders or talcum on the feet, and allowing shoes to dry in open air for twenty-four hours before wearing them.
Athlete’s foot usually returns due to the lack of preventive measures, failure to use antifungal medications as required and resistant fungi that fail to disappear even after thorough treatment. You can inhibit the condition by drying your feet after coming into contact with water, wearing open-toed shoes, wearing sock indoors, changing socks, wearing socks that can absorb sweat, using antifungal powders or talcum on the feet, and allowing shoes to dry in open air for twenty-four hours before wearing them.
What You Should Think About
If the symptoms are not bothersome or do not pose any health problems, you may decide not to cure athlete’s foot. However, remember that untreated cases that cause skin cracks and blisters can cause serious bacterial infections. Moreover, the disease can spread to others. Furthermore, sudden severe infections normally respond to treatment, unlike chronic infections.